BASIC INTERPRETATION OF THE LSCT
Note: This is part of a chapter in 'The Development of an evidenced-based submaximal cycle test designed to monitor and predict cycling performance' R.P. Lamberts (ISBN: 978-90-9024959-9) - please use this reference if you use info from this webpage. © Copyright 2009: R.P. Lamberts.
USING THE LSCT TO MONITOR FATIGUE AND CHANGES IN PERFORMANCE
A hypothetical model on how the LSCT reflects a change in training status and how measurements during the LSCT respond to acute and the chronic accumulation of fatigue is discussed below. This hypothetical model has been formulated based on the findings of the 6 studies of this thesis and the general principles of exercise physiology (Brooks et al. 2005).
Meaningful changes measured by the LSCT are defined by values which are higher than the normal day-to-day variation of those variables. These are shown in Table 8.1.
Table 8.1 An overview of meaningful changes of parameters measured by the LSCT.
|
|
|
Meaningful difference (absolute value)* |
|
Meaningful difference (Relative value)* |
|
Stage 1 Power |
|
≥ 18 W |
|
≥ 16% |
|
Speed |
|
≥ 3 km·h-1 |
|
≥ 8% |
|
Cadence |
|
≥ 7 rpm |
|
≥ 7% |
|
RPE |
|
≥ 2.0 units |
|
- |
|
Stage 2 Power (W) |
|
≥ 11 W |
|
≥ 6% |
|
Speed (km·h-1) |
|
≥ 2 km·h-1 |
|
≥ 3% |
|
Cadence (rpm) |
|
≥ 6 rpm |
|
≥ 7% |
|
RPE (units) |
|
≥ 2.0 units |
|
- |
|
Stage 3 Power (W) |
|
≥ 6 W |
|
≥ 3% |
|
Speed (km·h-1) |
|
≥ 2 km·h-1 |
|
≥ 3% |
|
Cadence (rpm) |
|
≥ 6 rpm |
|
≥ 6% |
|
RPE (units) |
|
≥ 2.0 units |
|
- |
|
Recovery HRR |
|
≥ 3 beats |
|
≥ 6% |
* Values are based on the study 5 (Lamberts et al. 2009a)
CHANGES IN MEASUREMENTS DURING THE LSCT WITH CHANGES IN TRAINING STATUS
The maximal heart rate and submaximal heart rate at high intensities remains relatively unchanged in professional cyclists throughout the season (Lucia et al. 2000), providing they do not become fatigued or over-trained. Based on the knowledge that peak power and submaximal power improves with an improvement in training status, and decreases with a decrease in training status (Brooks et al. 2005; Jeukendrup 2002), we expect that these changes also can be seen within the LSCT. Support for this hypothesis was found in Chapter 7, in which a cyclo-cross cyclist showed a similar improvement in PPO (24 W) and power output at 90% of HRmax (27 W) within the LSCT (Lamberts et al. 2009a). Additional support for this hypothesis was found in Chapter 6, in which a good correlation (r= 0.94) was found between PPO and power output at 90% of HRmax (Lamberts et al. 2009b). However, as Chapter 6 did not study whether a change in PPO is reflected in a change power output at 90% of HRmax and Chapter 7 describes a case study, future research needs to confirm this hypothesis. Hypothetically, assuming that submaximal power output changes with a change in training status, we expect this is reflected in the LSCT as follows (see also figure 8.1):
Improved training status:
· Higher power output especially during the second (≥ 6% or ≥ 11W) and third stage (≥ 3% or ≥ 6 W) of the LSCT
· A faster HRR (≥ 6% or ≥ 3 beats) after the third stage of the LSCT
· The same or similar RPE scores (within 1 unit).
Decrease in training status:
· Lower power output especially during second (≥ 6% or ≥ 11W) and third stage (≥ 3% or ≥ 6 W) of the LSCT
· A slower HRR (≥ 6% or 3 beats) after the third stage of the LSCT
· The same or similar RPE scores (within 1 unit).
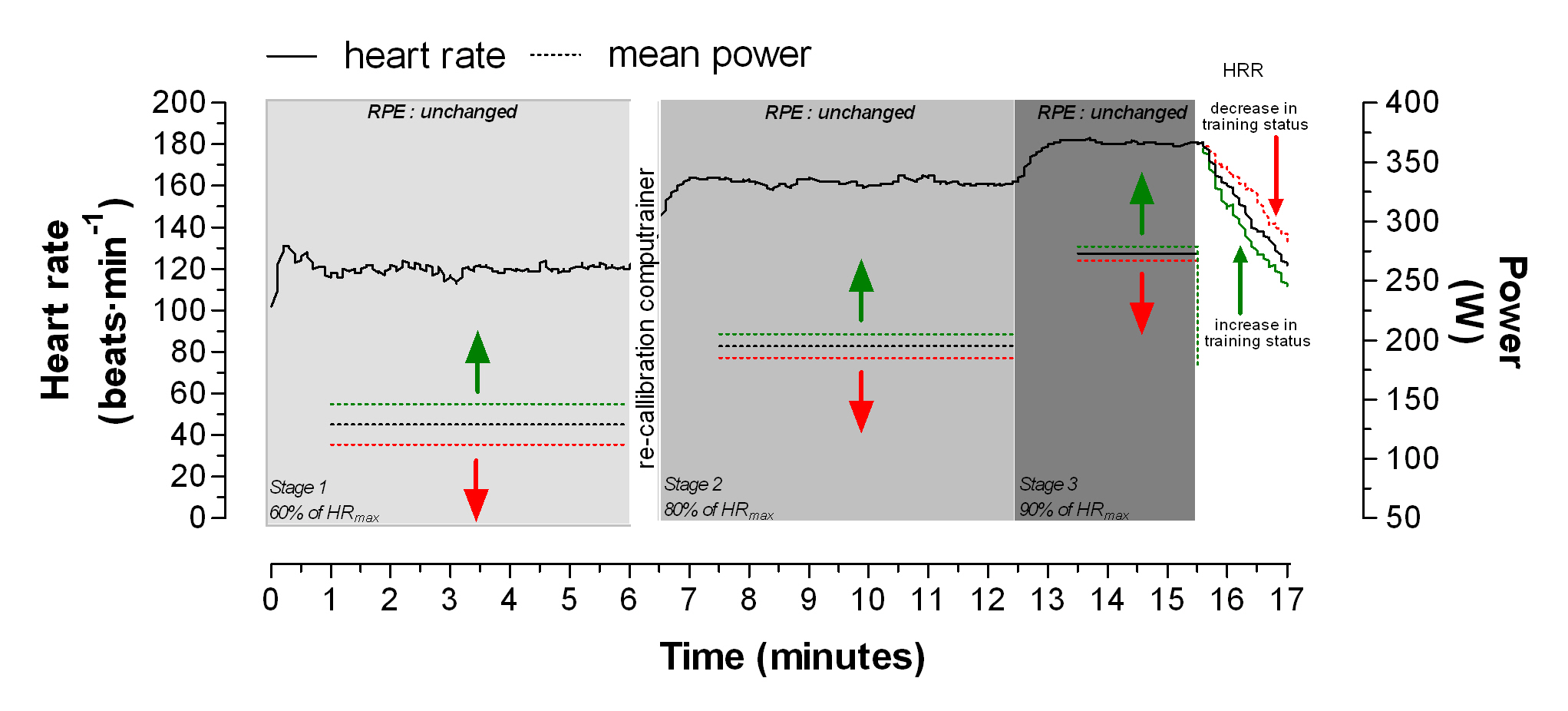
Figure 8.1 Graphical presentation of meaningful changes in power (W) and HRR response with either an improvement in training status (green arrows) or a decrease in training status (red arrows).
* The green and red dotted line during the first, second and third stage of the LSCT are represented by the TEM (Table 8.1) in the power measurement during these stages.
CHANGES IN THE LSCT WITH FATIGUE
As peak and submaximal power decreases with the accumulation of fatigue (Halson et al. 2002; Urhausen et al. 1998), it has been suggested that RPE levels increase with fatigue (Rietjens et al. 2005; Uusitalo et al. 1998) and HRR tracks with changes in training status (Sugawara et al. 2001). Therefore, the LSCT can possibly monitor the accumulating fatigue and possibly even assist with identifying a state of functional or non-functional overreaching. Although it is likely that additional tests such as a clinical assessment and a double maximum exertion test as described by Meeusen et al (2004) are needed to confirm a state of overreaching or overtraining, the LSCT seems to be a more practical tool for monitoring fatigue on a regular basis without interfering with their normal training habits.
Changes in the LSCT with the accumulation of acute fatigue and functional overreaching
In Chapter 7 a decrease in power output was seen at 60 and 80% of HRmax, while a stagnation in power output was seen at 90% of HRmax on two occasions. These decrements in performance were seen with an increased rating of perceived exertion and an increased heart rate recovery, which could reflect the accumulation of fatigue. However, the subject decreased his training load substantially in the following week, possibly allowing his body to recover and therefore power output, RPE and HRR returned to ‘normal’ values. As such a response shows similarities with a state of functional overreaching (Meeusen et al 2004), it is possible the observed responses within the LSCT are able to reflect this status. However as this was only a case study we want to emphasize that this is a hypothetical model which needs to be tested and confirmed in future research projects. However we hypothesize that the following adaptations will be seen within the LSCT with the accumulation of acute fatigue (see also Figure 8.2):
· Higher power outputs especially during second (≥ 6% or ≥ 11W) and first minute of third stage of the LSCT (≥ 3%
or ≥ 7 W *).
· A faster HRR (≥ 6% or ≥ 3 beats) after stage 3 of the LSCT.
· Increased RPE (≥ 2.0 units) during the second and third stage of the LSCT.
· Possibly not being able to reach the target HR of the third stage of the LSCT.
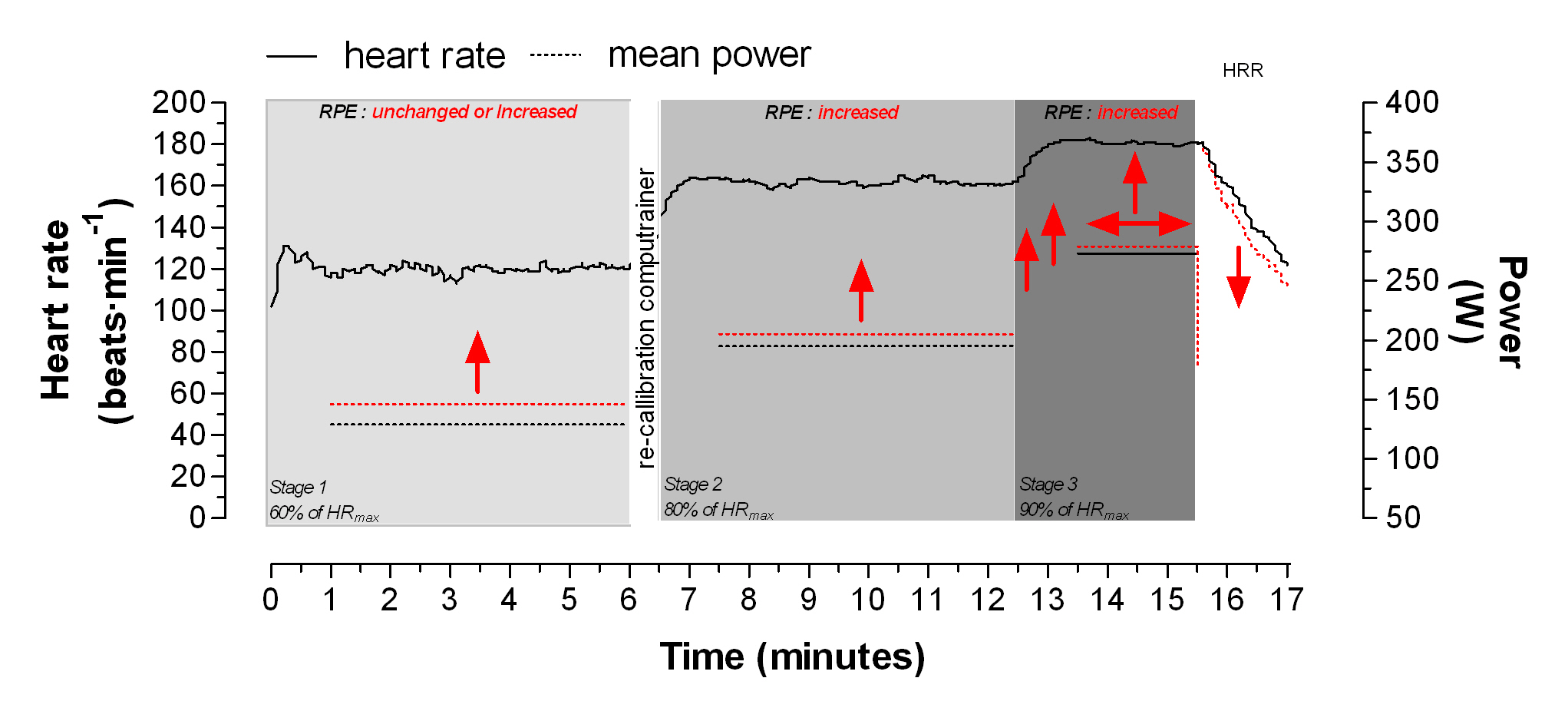 Figure 8.2 Graphical presentation of the responses from the LSCT to acute fatigue or possibly non-functional state of overreaching.
Figure 8.2 Graphical presentation of the responses from the LSCT to acute fatigue or possibly non-functional state of overreaching.
Changes in the LSCT with the manifestation of chronic fatigue and non-functional overreaching.
If the balance between training load and recovery persists the accumulation of fatigue becomes chronic and the decrement in performance progresses. Urhausen et al (1998) showed that endurance performance is initially affected while no changes in 10 and 30 second sprints were seen. This is in line with the blunted improvements in 40km TT power we documented in GDecr in Chapter 4. Although there were no real decreases in 40km TT power in GDecr, GIncr. improved significantly more in then GIncr. This blunted improvement could indicate the start of a stagnation or even a decrease in endurance performance in GDecr. This is supported by the decrease in HRR which has been associated with a decrease in training status (Sugawara et al. 2001). According to this explanation, we expect to see the following changes within the LSCT with the chronic manifestation of fatigue (see also Figure 8.3):
· Lower power outputs especially during the second (≥ 6% or ≥ 11W) and third stage (≥ 3% or ≥ 7 W) of the LSCT.
· A slower HRR (≤ 6% or ≤ 3 beats) after stage 3 of the LSCT.
· Increased RPE levels (≥ 2.0 units) during the second and third stage of the
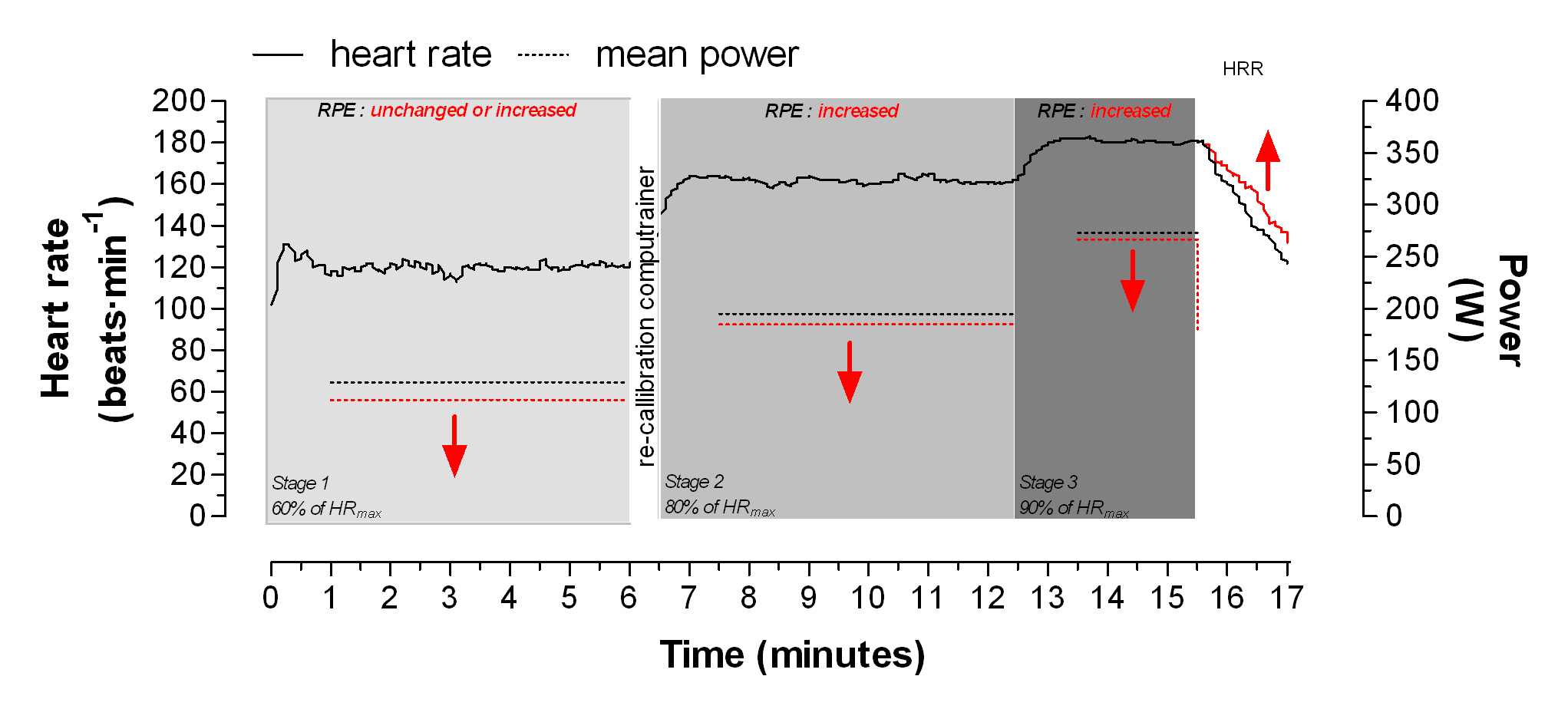
Figure 8.3 Proposed hypothesis on how the LSCT would reflect a state of chronic fatigue or possibly a non-functional state of overreaching.
* The scenario of not being able to reach the target heart rate during the third stage of the LSCT is not graphically displayed.
CONCLUSIONS
Based on the findings of the different studies within this thesis and research which is in accordance with other research findings (Brooks et al. 2005; Buchheit et al. 2007b; Buchheit et al. 2007a; Buchheit et al. 2008; Halson et al. 2002; Halson and Jeukendrup 2004; Jeukendrup 2002; Lehmann et al. 1998; Lehmann et al. 1997; Meeusen et al. 2004; Rietjens et al. 2005; Rushall 1990; Sugawara et al. 2001; Uusitalo et al. 1998), we conclude that the LSCT has the potential to monitor changes in training status on a regular basis.However, it seems highly unlikely that only one parameter can consistently and accurately indicate acute fatigue or predict the accumulation of fatigue. Therefore we find it prudent to suggest that rather than focus on a single predictor, a combination of parameters should be used to monitor changes in training status and to predict the accumulation of fatigue. In particular the combination of an objective data source (i.e. measurement of power), an subjective data source ((i.e. rating of perceived exertion) and alterations in the functioning of the autonomic nervous sustem (measured by HRR) shows advantages over measuring just one variable source. Future research needs to determine which combination of these parameters reflects particular changes in training status and/or indicates the accumulation of fatigue.
In conclusion, the LSCT shows potential to monitor and predict changes in training status and possibly can play an important role in reflecting fatigue levels. This can have important practical implications for scientists and coaches who can use this information to optimize training programs and diagnose states of non-functional and functional overreaching at an early stage.
In an attempt to assist with decision-making and the interpretation of data measured during the LSCT, a scheme is proposed in Table 8.2. This scheme is hypothetical based on the data presented in this thesis. Further research needs to test the accuracy and practical application of the model.
Table 8.2 A basic scheme to describe the decision-making of adjusting training load ,based on the change in performance parameters measured within the LSCT
|
Amount of changes within LSCT parameters |
Description |
Examples # |
Recommendation |
|
0 |
No changes one of the LSCT parameters in HRR, power output and RPE. |
·No change in HRR, power outputs* and RPE levels**
|
No indication of accumulation of fatigue.
Keep on training
|
|
1 |
Change in one of the LSCT parameters HRR, power output or RPE |
·A faster HRR with no change in power outputs* and RPE levels** ·Change in RPE levels** scores without a change in power outputs* and HRR ·Change in power outputs* without a change in HRR and RPE levels**
|
Unlikely risk for the accumulation of fatigue
No direct indication for the accumulation of fatigue.
Carefully monitor symptoms |
|
2 |
Change in two of the LSCT parameters HRR, power output or RPE |
·A faster HRR with an increase power output* but no change in RPE levels** ·A slower HRR with increased RPE levels** but no change in power output* ·A slower HRR with decrease in power outputs but no change in RPE levels
|
Likely risk for the accumulation of fatigue
Adapt training protocol and monitor symptoms.
(lower training load and/or increase recovery period)
|
|
3 |
Change in all of the LSCT parameters HRR, power output and RPE |
·A slower HRR with increased RPE levels and a decrease in power output · A faster HRR with an increase in power during the first minute of the third stage and increased RPE levels. |
Highly likely risk of the accumulation of fatigue with detrimental effects on performance.
Adapt training protocol !!
(minimize training load or increase recovery time)
|
# These are examples, not all possible scenarios are given * Meaningful change in power output during stage 2 and 3 and the first minute of the stage 3. ** Meaningful change in RPE during stage 2 and 3.
Although heart rate recovery (HRR), was selected as one of the main outcome measures, based on the papers of Buchheit et al. (2007b; 2008), the measurement of heart rate variability (HRV) also shows the potential of being a useful marker in monitoring fatigue and changes in training status. However, as there is no consensus on how to analyze HRV data, judgements about the practical value of HRV analysis seem to be premature and difficult to make at this stage. However when consensus is reached on how to analyse HRV data, this information can possibly be added as a valuable extra component to the LSCT.
REFERENCES
Baumert M, Brechtel L, Lock J, Hermsdorf M, Wolff R, Baier V and Voss A (2006) Heart rate variability, blood pressure variability, and baroreflex sensitivity in overtrained athletes. Clin J Sport Med 16: 412-417
Brooks GD, Fahey TD and Baldwin KM(2005) Exercise Physiology: Human Bioenergetics and Its Applications. McGraw-Hill, New York, NY.
Buchheit M, Laursen PB and Ahmaidi S (2007a) Parasympathetic reactivation after repeated sprint exercise. Am J Physiol Heart Circ Physiol 293: H133-H141
Buchheit M, Millet GP, Parisy A, Pourchez S, Laursen PB and Ahmaidi S (2008) Supramaximal training and postexercise parasympathetic reactivation in adolescents. Med Sci Sports Exerc 40: 362-371
Buchheit M, Papelier Y, Laursen PB and Ahmaidi S (2007b) Noninvasive assessment of cardiac parasympathetic function: postexercise heart rate recovery or heart rate variability? Am J Physiol Heart Circ Physiol 293: H8-H10
Bunc V, Heller J and Leso J (1988) Kinetics of heart rate responses to exercise. J Sports Sci 6: 39-48
Currell K and Jeukendrup AE (2008) Validity, reliability and sensitivity of measures of sporting performance. Sports Med 38: 297-316
Esteve-Lanao J, Foster C, Seiler S and Lucia A (2007) Impact of training intensity distribution on performance in endurance athletes. J Strength Cond Res 21: 943-949
Halson SL, Bridge MW, Meeusen R, Busschaert B, Gleeson M, Jones DA and Jeukendrup AE (2002) Time course of performance changes and fatigue markers during intensified training in trained cyclists. J Appl Physiol 93: 947-956
Halson SL and Jeukendrup AE (2004) Does overtraining exist? An analysis of overreaching and overtraining research. Sports Med 34: 967-981
Jeukendrup A(2002) High-performance cycling. Human Kinetics Publishers, Inc., Champaign, IL, USA.
Kenttä G and Hassmén P (1998) Overtraining and recovery. A conceptual model. Sports Med 26: 1-16
Lamberts RP, Rietjens G.J., Tijdink HH, Noakes TD and Lambert MI (2009a) Measuring submaximal performance parameters to monitor fatigue and predict cycling performance: a case study of a world-class cyclo-cross cyclist. Eur J Appl Physiol Epub; ahead of publication.
Lamberts RP, Swart J, Noakes TD and Lambert MI (2009b) A novel submaximal cycle test to monitor fatigue and predict cycling performance. Br J Sports Med Epub; ahead of publication.
Lamberts RP, Swart J, Noakes TD and Lambert MI (2009c) Changes in heart rate recovery after high-intensity training in well-trained cyclists. Eur J Appl Physiol 105: 705-713
Lamberts RP, Swart J, Noakes TD and Lambert MI (2009d) Heart rate recovery as a guide to monitor fatigue and predict changes in performance parameters. Scand J Med Sci Sports Epub; ahead of publication.
Laursen PB and Jenkins DG (2002) The scientific basis for high-intensity interval training: optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med 32: 53-73
Laursen PB, Shing CM, Peake JM, Coombes JS and Jenkins DG (2002) Interval training program optimization in highly trained endurance cyclists. Med Sci Sports Exerc 34: 1801-1807
Lehmann M, Foster C, Dickhuth HH and Gastmann U (1998) Autonomic imbalance hypothesis and overtraining syndrome. Med Sci Sports Exerc 30: 1140-1145
Lehmann MJ, Lormes W, Opitz-Gress A, Steinacker JM, Netzer N, Foster C and Gastmann U (1997) Training and overtraining: an overview and experimental results in endurance sports. J Sports Med Phys Fitness 37: 7-17
Lucia A, Hoyos J, Perez M and Chicharro JL (2000) Heart rate and performance parameters in elite cyclists: a longitudinal study. Med Sci Sports Exerc 32: 1777-1782
Meeusen R, Duclos M, Gleeson M, Rietjens GJ, Steinacker JM and Urhausen A (2006) Prevention, diagnosis and treatment of the overtraining syndrome. Eur J Sport Sci 6: 1-14
Meeusen R, Piacentini MF, Busschaert B, Buyse L, De Schutter G and Stray-Gundersen J (2004) Hormonal responses in athletes: the use of a two bout exercise protocol to detect subtle differences in (over)training status. Eur J Appl Physiol 91: 140-146
Meyer T, Auracher M, Heeg K, Urhausen A and Kindermann W (2007) Effectiveness of low-intensity endurance training. Int J Sports Med 28: 33-39
Paton CD and Hopkins WG (2001) Tests of cycling performance. Sports Med 31: 489-496
Paton CD and Hopkins WG (2006) Ergometer error and biological variation in power output in a performance test with three cycle ergometers. Int J Sports Med 27: 444-447
Pichot V, Busso T, Roche F, Garet M, Costes F, Duverney D, Lacour JR and Barthelemy JC (2002) Autonomic adaptations to intensive and overload training periods: a laboratory study. Med Sci Sports Exerc 34: 1660-1666
Rietjens GJ, Kuipers H, Adam JJ, Saris WH, van Breda E, van Hamont D and Keizer HA (2005) Physiological, biochemical and psychological markers of strenuous training-induced fatigue. Int J Sports Med 26: 16-26
Rushall BS (1990) A Tool for Measuring Stress Tolerance in Elite Athletes. Journal of Applied Sport Psychology 2: 51-66
Seiler KS and Kjerland GO (2006) Quantifying training intensity distribution in elite endurance athletes: is there evidence for an "optimal" distribution? Scand J Med Sci Sports 16: 49-56
Short KR and Sedlock DA (1997) Excess postexercise oxygen consumption and recovery rate in trained and untrained subjects. J Appl Physiol 83: 153-159
Stepto NK, Hawley JA, Dennis SC and Hopkins WG (1999) Effects of different interval-training programs on cycling time-trial performance. Med Sci Sports Exerc 31: 736-741
Sugawara J, Murakami H, Maeda S, Kuno S and Matsuda M (2001) Change in post-exercise vagal reactivation with exercise training and detraining in young men. Eur J Appl Physiol 85: 259-263
Urhausen A, Gabriel HH, Weiler B and Kindermann W (1998) Ergometric and psychological findings during overtraining: a long-term follow-up study in endurance athletes. Int J Sports Med 19: 114-120
Uusitalo AL, Uusitalo AJ and Rusko HK (1998) Exhaustive endurance training for 6-9 weeks did not induce changes in intrinsic heart rate and cardiac autonomic modulation in female athletes. Int J Sports Med 19: 532-540
